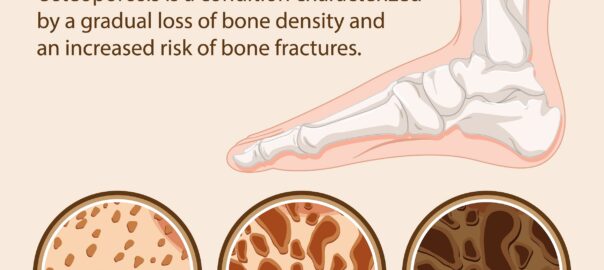
Osteoporosis, a condition characterized by low bone density and increased risk of fractures, can have significant implications for podiatric care. The bones of the feet and ankles are not immune to the effects of osteoporosis, and podiatrists play a crucial role in both the prevention and management of foot-related issues associated with this condition.
Call housecall podiatrists at Chicago Home Foot Care at 312-998-0974. Our Chicago podiatrists can provide a proper diagnosis based on your symptoms, medical history, and potentially recommend imaging studies or other diagnostic tests to identify the underlying cause and determine the appropriate treatment.
Here are several ways in which osteoporosis intersects with podiatry:
- Fracture Risk Assessment: Podiatrists may assess patients with osteoporosis for their risk of foot and ankle fractures. Individuals with osteoporosis are at increased risk of stress fractures, particularly in weight-bearing bones such as the calcaneus (heel bone) and metatarsals (bones of the midfoot).
- Footwear Recommendations: Podiatrists may provide guidance on appropriate footwear for individuals with osteoporosis. Shoes with good support, cushioning, and stability can help reduce the risk of falls and fractures, especially in those with weakened bones.
- Fall Prevention Strategies: Podiatrists can educate patients with osteoporosis about strategies to prevent falls, which can significantly reduce the risk of fractures. This may include exercises to improve balance and strength, as well as removing hazards in the home environment.
- Orthotic Devices: Custom orthotic devices may be prescribed by podiatrists to help redistribute pressure away from vulnerable areas of the foot, reducing the risk of developing ulcers or stress fractures, especially in individuals with osteoporosis-related foot deformities.
- Management of Foot Deformities: Osteoporosis can contribute to foot deformities such as bunions, hammertoes, and Charcot foot. Podiatrists can provide conservative treatments such as orthotics, padding, and footwear modifications to alleviate symptoms and prevent further complications.
- Wound Care: Individuals with osteoporosis are at increased risk of foot wounds due to decreased bone density and altered biomechanics. Podiatrists play a vital role in the management of foot ulcers, including debridement, offloading, and wound dressings, to prevent infection and promote healing.
- Collaborative Care: Podiatrists often work closely with other healthcare professionals involved in the care of patients with osteoporosis, such as primary care physicians, orthopedic surgeons, and physical therapists, to ensure comprehensive management and optimal outcomes.
Overall, podiatrists play a critical role in the prevention, assessment, and management of foot-related issues in individuals with osteoporosis, helping to improve mobility, reduce pain, and enhance quality of life.